Bleeding in human childbirth
Vaginal delivery: ˂ 500 ml
Caesarean section: ˂1000 ml
2017 - revision of the definition of PPH
- blood loss > 500 ml vaginal delivery
or
- blood loss >1 000 ml Caesarean section
or
- change in vital functions
- heart rate >15% ≥110 bpm,
- blood pressure ≤ 85/45 mmHg,
- saturation < 95%
There is strength in simplicity…
An acute, life-threatening condition
Peripartum haemorrhage – definition Czech Republic
According to the amount of blood loss:
- minor blood loss (500 – 1 000 ml)
- severe blood loss (> 1 000 ml)
- life-threatening peripartum hemorrhage (LTPPH) (> 1 500 ml)
(clinical and/or laboratory signs of tissue hypoperfusion)


Incidence 7-8%
The incidence of LTPPH/PPH varies greatly depending on the criteria used to diagnose the pathology.
Estimate: 1 - 5% of births
Sheldon WR, Blum J, Vogel JP, et al. Postpartum haemorrhage management, risks, and maternal outcomes: findings from the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG 2014; 121 Suppl 1:5.
Reale SC, Easter SR, Xu X, et al. Trends in Postpartum Hemorrhage in the United States From 2010 to 2014. Anesth Analg 2020; 130:e119.
Prospective study: 10% of births
Deneux-Tharaux C, Bonnet MP, Tort J. [Epidemiologie poporodního krvácení ]. J Gynecol Obstet Biol Reprod (Paříž) 2014; 43: 936.
Physiology of postpartum haemostasis
Woman
- pregnant woman
- 2nd half of pregnancy

Haemostasis mechanism
=
combination of two factors
Mechanical haemostasis
- retraction of the myometrium → compression = tourniquet of the vascular system of the uterus
Coagulation haemostasis
- decidual/tissue factors
- plasminogen activator type 1 inhibitor
- systemic coagulation factors (circulating haemostasis factors, platelets, etc.)
Pathogenesis of most cases of PPH = disruption of one or both mechanisms.
Pathogenesis of other cases of PPH is loss of intact vasculature (i.e. trauma).


LTPPH DIC
95% 5%
Physiology of retraction-tourniquet myometrium
- perfusion
- oxygenation
- energy reserves
- receptor readiness
Risk factors Specific etiology
Study (690,000 births): 4 risk factors associated with the highest probability of
predicting
the need for massive blood transfusion (n = 406) during hospitalization for
delivery
Mhyre JM, Shilkrut A, Kuklina EV, et al. Massive blood transfusion during hospitalization for delivery in New
York State, 1998-2007. Obstet Gynecol 2013; 122:1288.
- abnormal placentation (pl. accreta or previa) (1.6/10,000 births, OR 18.5, 95% CI 14.7-23.3)
- placental abruption (1.0/10,000 births, OR 14.6, 95% CI 11.2-19.0)
- severe preeclampsia (0.8/10,000 births, OR 10.4, 95% CI 7.7–14.2)
- intrauterine fetal death (0.7/10,000 births, OR 5.5, 95% CI 3.9–7.8)
Other risk factors for PPH
personal or family history of previous PPH, obesity, multiparity, Asian or Hispanic race, precipitous delivery, excessive uterine distention (e.g. multiple pregnancy, polyhydramnios, fetal macrosomia), chorioamnionitis, uterine inversion, uterine fibroids, Couvelair uterus, inherited bleeding diathesis, acquired bleeding diathesis (e.g. amniotic fluid embolism, abruptio placentae, sepsis, fetal death), assisted reproduction technology, anaemia and the use of certain drugs: muscle relaxants, antithrombotics.
ANTIDEPRESSANTS, especially selective serotonin reuptake inhibitors (SSRIs) and serotonin and noradrenaline reuptake inhibitors (SNRIs) - ANAEMIA
Preventive measures
Recommendation
We recommend treatment of antenatal anaemia. Pregnant women should be given iron preparations if their hemoglobin level falls below 110g/l in the first trimester or below 105g/l in the 28th week of pregnancy.
Recommendation
We suggest considering parenteral iron in women with sideropenic anaemia unresponsive to oral iron supplementation.
Life-threatening peripartum haemorrhage
Anamnesis
Risk factors 40%
A.
- multiple pregnancy
- preeclampsia/gestational hypertension
- placenta praevia
- suspected premature separation of the placenta
- suspected amniotic fluid embolism
B.
- Life-threatening peripartum haemorrhage in previous childbirth
- Asians
- Obesity (BMI > 35)
- Anaemia (< 9g/ml)
C.
- Acute Caesarean section
- Induction of labour
- Placenta adhaerens
- Operative vaginal delivery
- Prolonged labour (> 12 hours)
- Large fetus (> 4 kg)
- Fever during labour
- Morther's age (> 40 years)
Risk Factors 60%


Preventive measures
Recommendation
Women with risk factors for life-threatening PPH should give birth in medical facilities appropriately staffed and materially equipped to deal with life-threatening PPH.
Recommendation
For patients with a high risk of PCOS (abnormal placentation), we recommend formulating a care plan with the participation of a multidisciplinary team in a reasonable time before delivery.
Bleeding in human childbirth
Before delivery - DIC, Life-threatening PPH
- placental abruption
- amnioticfluid embolism
- endo/myometritis
- preeclampsia/HELLP
During delivery - Life-threatening PPH, DIC
- in III. stage of labour (delivery of the placenta)
- during the operation
After delivery - Life-threatening PPH
- hysterotomy
4 T
Disorders of uterine Tonus 70 – 80%
- postpartum uterine hypo-/atony

Birth Trauma 10 – 15%
- laceration of the cervix, vagina, perineum
- pelvic haematomas
- uterine rupture, intraoperative complications
- inversion of the uterus
Trauma related to bleeding
= tissue laceration (including uterine rupture) or surgical incisions.
Lacerations/ruptures of the cervix and vagina will be caused by
- fetus – passage through the birth canal
- assistance - intervention during childbirth
Lacerations/ruptures
- obvious
- hidden (haematomas of the vulva, paracolpia, retroperitoneum)
Tissue pathology 1 – 5%
- placenta adherens, placenta accreta
Coagulopathy (Thrombin) 1 – 5%
- DIC early (amniotic fluid embolism, abruption!!!)
Coagulopathy (Thrombin)
- about 1 in 500 births in the U.S.
- < 7% of PPH cases (placental abruption, amniotic fluid embolism)
Reale SC, Easter SR, Xu X, et al. Trends in Postpartum Hemorrhage in the United States From 2010 to 2014. Anesth Analg 2020; 130:e119. - Congenital coagulopathies
von Willebrand disease = high risk of PPH- von Willebrand factor level during pregnancy ↑, after delivery ↓↓↓
- Acutely acquired coagulopathy
- amniotic fluid embolism
- placental abruption
- severe preeclampsia
- < 7% of PPH cases (placental abruption, amniotic fluid embolism)
- HELLP syndrome (haemolysis, elevated liver enzymes, low platelets)

Causes of PPH
Disorders of uterine tonus 70 – 80%
- postpartum uterine hypo-/atony
Delivery trauma 10 – 15%
- laceration of the cervix, vagina, perineum
- pelvic haematomas
- uterine rupture, intraoperative complications
- uterus inversion
Tissue pathology 1 – 5%
- placenta adherens, placenta accreta
Coagulopathy 1 – 5%
- DIC early (amniotic fluid embolism, abruption!!!)
Clinical note:
During pregnancy, a woman's blood volume increases physiologically, where at the end of pregnancy the increase is up to 40% of the original volume.
Initial symptoms of a haemorrhagic shock are therefore less pronounced during pregnancy.
As long as the blood loss does not exceed 1000 ml, the systemic pressure and the heart rate of the pregnant/partum/six-weeks-postpartum woman are maintained within the physiological range.


Causes of non-standard care for a woman with PPH
- delayed diagnosis
- delayed treatment due to underestimated blood loss
- delayed preparation of blood products and coagulation factors
- lack of management protocols
- insufficient professional training of personnel
- poor communication between the interdisciplinary team
- deficiencies in organization and delays in initiation of treatment
Reduction of maternal mortality and morbidity
- timely identification of PPH
- timely and correct diagnosis of the cause of bleeding
- rapid intervention/treatment of PPH
High risk of excessive bleeding during delivery
- III. stage of labour = myometrial perfusion 600 ml/min. about 15% of the mother's cardiac output
- Haemostasis = after delivery of the placenta
Life-threatening peripartum bleeding
When? = start (time)
Where? = localization
How? = amount
Management of life threatening
peripartum haemorrhage – applies !!!
- rapid anti-shock measures
- rapid surgical treatment
- .rapid intensivist treatment = substitution of blood factors

Real time
- collection time
- time required for transport to the laboratory
- material processing
- result available…..???

We recommend monitoring coagulation and the initiation of measures to adjust coagulations as soon as possible
after identifying the condition of life-threatening PPH.
To identify the type of coagulation disorder in life-threatening PPH we recommend using viscoelastometric methods (TEG, ROTEM), if available.
Recommendation
We recommend fibrinogen substitution in patients with life-threatening PPH when its level drops below 2 g/l and/or when its functional deficit is detected by viscoelastometric methods or when there is a justified clinical assumption of fibrinogen deficiency even without knowledge of its levels.
As a minimum initial dose for life-threatening PPH, we recommend the administration of an initial dose of at least 3 g (4 g) of fibrinogen or the equivalent of this dose when using transfusion preparations with increased fibrinogen content.
Recommendation
We recommend prophylactic administration of uterotonics in III. stage of labour immediately after the birth of the child before ligation of the umbilical cord. The drug of first choice is oxytocin.
Recommendation
We suggest considering the administration of carbetocin in women with an increased risk of life-threatening PPH.
Recommendation
For women with an increased risk of life-threatening PPH undergoing Caesarean section, we suggest considering a single administration of tranexamic acid (TXA) along with carbetocin.
Midwife
- statim mask for oxygen supply
- IV securing with a strong cannula
- permanent urinary catheter
Doctor
ANAMNESIS - informed by the midwife
- inquiry about the suspected cause of bleeding
- blood loss estimation query
- Monitoring of BP, P, saturation
- BP falls and heart rate rises
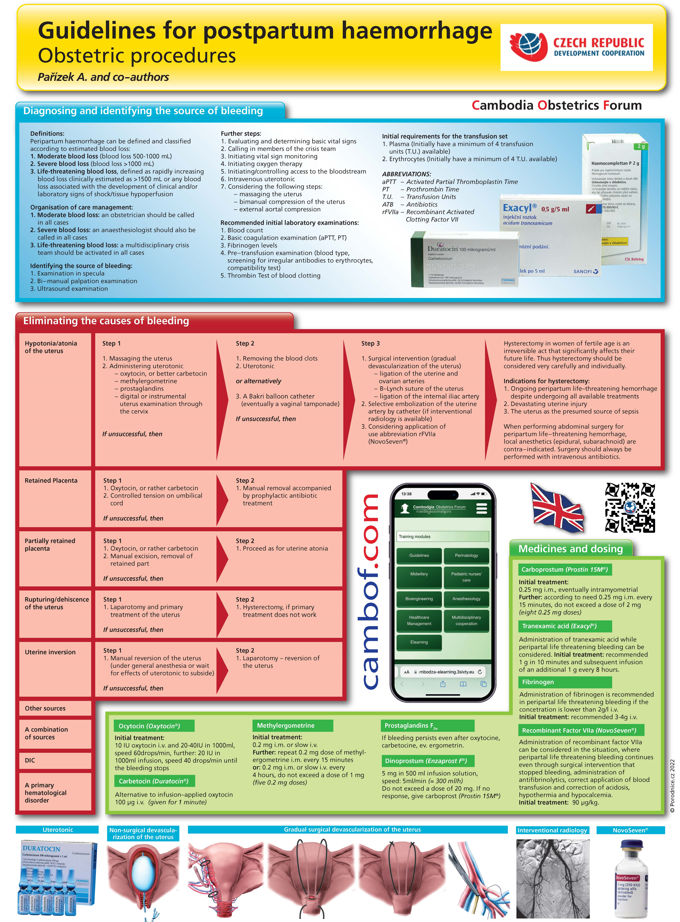
Identifying the source of bleeding:
- examination in mirrors
- palpation bimanual examination
- ultrasound examination
Differential diagnostics
- uterine hypotonia/atony
- retention of the placenta
- retention of part of the placenta
- uterine rupture/dehiscence
- uterus inversion
- birth canal injury
- DIC (PLT, APTT, PT, fibrinogen, D-dimers, antithrombin)
- primarily haematological disorder
The doctor checks the previous procedures:
- assessment and provision of basic life functions
- initiation of monitoring of basic vital functions
- initiation of oxygen therapy
- ensuring/controlling entry into the bloodstream
- initiation of fluid replacement/fluid resuscitation
- IV administration of uterotonics
He will recommend an initial laboratory examination:
- blood count
- basic coagulation examination (aPTT, PT)
- fibrinogen level
- pre-transfusion examination (blood group, screening for irregular antibodies against erythrocytes, compatibility test)
- orientation test of blood clotting with thrombin
Initial requirements for transfusion products:
- plasma (in the initial phase of ensuring the availability of at least 4 transfusion units)
- erythrocytes (in the initial phase of ensuring the availability of at least 4 transfusion units)
Uterine hypotonia/atony
Step 1
- uterine massage
- uterotonics
- oxytocin, better carbetocin
- methylergometrine
- prostaglandins
- digital or instrumental revision of the uterine cavity
In case of failure - Step 2
- removal of coagulum
- uterotonics
- Bakri balloon catheter, (eventual vaginal tamponade)
In case of failure, immediately - Step 3.
- surgical intervention (gradual devascularization of the uterus)
- ligation aa. uterinae and aa. ovaricae
- B-Lynch uterine suture
- ligation aa. iliacae internae
2. selective catheter embolization aa. uterinae (if interventional radiology is available)
3. consideration of administration of recombinant activated factor VII (NovoSeven®)
Coagulation support
General principles
Basic initial procedures to restore the effectiveness of the body‘s
hemostatic mechanisms and to support coagulation:
- maximum possible correction of hypothermia
- maximum possible correction of acidosis
- correction of hypocalcemia
- correction of other system homeostasis parameters
- fibrinogen
- tranexamic acid
Ensuring/control of entry into circulation (insertion of at least 2 peripheral catheters with the largest possible diameter is recommended)
Initiate/continue fluid resuscitation (crystalloids and/or colloids)
- crystalloids, balanced solutions are preferred, the usual starting dose is approx. 2000 ml
- colloids, usual starting dose 500-1000 ml
Medicines and their dosage
Oxytocin (Oxytocin®)
Initiation of treatment: 10 IU i.m. and 20-40 IU in 1000 ml infusion solution, rate: 60 drops/min,
further: 20 IU in 1000 ml of infusion solution.
Rate: 40 drops/min, until bleeding stops.
Carbetocin (Duratocin®)
Replacement of oxytocin infusion 100 μg IV (administration time 1 minute)
Methylergometrine
Initiation of treatment: 0.2 mg i.m. or slowly i.v.
further: after 15 minutes, repeat administration of 0.2 mg methylergometrine i.m. r: 0.2 mg i.m. or slowly i.v. every 4 hours, do not exceed a dose of 1 mg (five doses of 0.2 mg)
Tranexamic acid (Exacyl®)
Initial dose 1 g in 10 minutes,
further: continue infusion at a dose of 1 g during 8 hours.
An alternative is a dosage of 20-25 mg/kg.
Fibrinogen'
The administration of fibrinogen is recommended for life-threatening PPH when its concentration drops below 2 g/l i.v.
Initial dose: for life-threatening PPH, 3 – 4 g i.v. is recommended.
Prostaglandins F2α
If bleeding continues even after administration of oxytocin, carbetocin, or ergometrine, prostaglandins are in order.
Dinoprost (Enzaprost F®)
5 mg in 500 ml of infusion solution, rate: 5 ml/min (= 300 ml/h) do not exceed a dose of 20 mg, if there is no response, give carboprost (Prostin 15M®).
Carboprost (Prostin 15M®)
Initiation of treatment: 0.25 mg i.m. alternatively intramyometrially,
further: as needed every 15 minutes 0.25 mg i.m., do not exceed a dose of 2 mg (eight doses of 0.25 mg).
Erythrocytes
- the target hemoglobin value is recommended to be at least 70 g/l (significant anaemia reduces the effectiveness of haemostasis mechanisms)
- recommended ratio of the number of TU erythrocytes and plasma is 1:1 to 1.5:1
Plasma
- administration of plasma is recommended for clinical signs of bleeding and prolongation of PT and/or aPTT to 1.5 times normal values or more
- the recommended minimum initial dose of plasma for life-threatening PPH is 15-20 ml/kg
Platelets
- administration of platelets is recommended for life-threatening PPH when the number of platelets drops below 70 x 109/l
The role of interventional radiology
In all cases of peripartum life-threatening bleeding due to hypotony or atony of the uterus, we recommend using radiological interventional methods (selective embolization of the uterine arteries), if available, when the usual standard surgical procedures fail (or are impossible to perform) in the workplace.




Morbidity and mortality
Mortality of PPH approx. 2% (large differences worldwide)
- 0.6% Great Britain
- 20% in some parts of Afric
Transfusion Women Trial (study of approx. 20,000 women)
- 54% blood transfusion
Risks of transfusion infection, abnormalities of
electrolytes, allergic reactions, alloimmunization
Hysterectomy (Women Trial)
- 3.5% of women hysterectomies postpartum for PPH
- USA 2014 hysterectomy 2.1% of women with PPH(atony 60%
- Czech Republic
Thromboembolism (Women Trial)
- 0.3% of women with PPH have a thromboembolic event within 42 days after birth.
Haemodynamic instability and organ failure (Women Trial)
- 4% kidney, heart, respiratory, liver failure
Sheehan syndrome
- postpartum hypopituitarism rare but potentially life-threatening complications
Abdominal compartment syndrome
- organ dysfunction caused by intra-abdominal hypertension is a rare but life-threatening complication of PPH with intra-abdominal bleeding
Asherman syndrome
- up to 90% of cases of severe intrauterine adhesions is related to revision/curettage of the uterus
Postpartum anaemia
- postpartum anaemia is commo
Recurrence
Women with previous PPH have up to an 18% risk of recurrence in subsequent pregnancy.
Oberg AS, Hernandez-Diaz S, Palmsten K, et al. Patterns of recurrence of postpartum hemorrhage in a large population- based cohort. Am J Obstet Gynecol 2014; 210:229.e1.
Ford JB, Roberts CL, Bell JC, et al. Postpartum haemorrhage occurrence and recurrence: a population-based study. Med J Aust 2007; 187:391.
Ruiter L, Kazemier BM, Mol BWJ, Pajkrt E. Incidence and recurrence rate of postpartum hemorrhage and manual removal of the placenta: A longitudinal linked national cohort study in The Netherlands. Eur J Obstet Gynecol Reprod Biol 2019; 238:114.

Conclusion
Recommended practices
Life-threatening PPH treatment principle
Myometrial Perfusion Oxygenation Uterotonics Plasma factors



Why drill in obstetrics…???
- very few opportunities for exposure to acute conditions
- very little personal experience
- practicing a series of procedures in planned simulated
- event is the only means of education (especially in obstetrics)
Proper management:
- saving your own skin





Peripartum haemorrhage
What needs to be available:
- knowledge
- elaborate procedures
- necessary medication
- technology – operative, intensiviste



Simulation Centre